Diabetic osteoneuropathy, also known as Charcot foot, is a comorbidity of up to 7.5% of diabetic patients with neuropathy. One third of these patients have problems with both feet.
Most patients have had poorly controlled diabetes for 15 to 20 years by the time we see the degeneration of the joint and bone loss, causing the deformity. We suspect that these numbers are low, because it is easy for doctors to overlook the progression of Charcot foot. The acute stage mimics cellulite and the chronic condition resembles osteomyelitis, which are also common diabetic comorbidities.
What is Charcot Foot and what causes it?
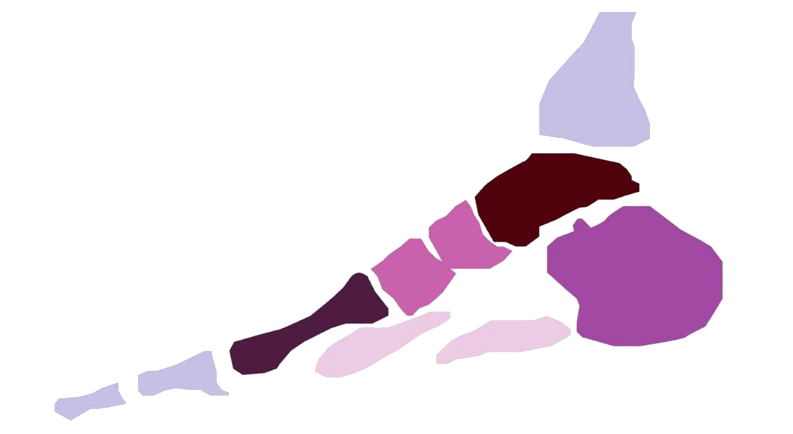
Charcot's foot begins with some type of micro-trauma, which triggers uncontrollable inflammation and nerve damage known as neuropathy. An increase in BMI with uncontrolled diabetes over a long period of time can also be a trigger for this condition. Pro-inflammatory cytokines trigger bone and joint destruction, causing the foot to fracture or the arch to collapse and distort into a bony prominence at the medial joint, commonly known as rocker foot. The foot is hot, swollen with fluid, hot to the touch, dry, and may or may not occur along with pain.
One modern theory is that Charcot foot is triggered by repetitive mechanical trauma to the feet. Up to 50% of patients recall a sprained ankle or a previous foot procedure. The second theory is that muscle imbalances produce an eccentric load on the foot, causing microfractures, loose ligaments, and bone degradation.
How is Charcot's foot diagnosed?
A key point in the diagnosis is the patient's amnamnesis. When we take a clinical history of our patient we must know all the pathologies that he presents, the treatments, his lifestyle, etc. because this will give us detailed information about what we are facing. It is very important to know the pathology and how it is treated, and if we suspect that the patient has Charcot foot, we should refer him to the endocrinologist and have an MRI done, since conventional radiology can overlook the subchondral edema of the bone marrow common to the disease. Of course, bone marrow edema could also mean arthritis, gout, or bone infection. Microfractures are also more visible on MRI scans, increasing the likelihood of a positive diagnosis.
If a patient with diabetic neuropathy has no history of ulceration and the foot has swollen, hot, and red skin, there is a good chance of Charcot foot. In patients with existing ulcers, a bone culture may be needed to confirm or deny Charcot's foot.
Phases and treatments
It depends on the phase in which the patient comes to the consultation will be in our hands to deal with one treatment or another. But we must not deny that this pathology cannot be. When the injury is presented in the early stages, the patient is asked to rest and not to support the affected member. For this purpose, the leg can be plastered to avoid wandering and deformity.
In more advanced stages can present in plantar area ulceration by support, so we will take special care to make discharges from the area of support and ulcerated and if you have injury will be made cures.
In very extreme cases, surgery can be performed on the bony area of the foot.
It is very important in a diabetic to have a period of assistance to their medical service and preventive care to avoid diagnosing the pathology in very advanced stages. For this reason, it is recommended that you go to your appointments with the nurse, carry out an analysis measuring the glycosylated haemoglobin values when your doctor considers it appropriate and a continuous visit to the chiropodist.

Comments